Infectious Diseases Case of the Month Case #24 |
|||
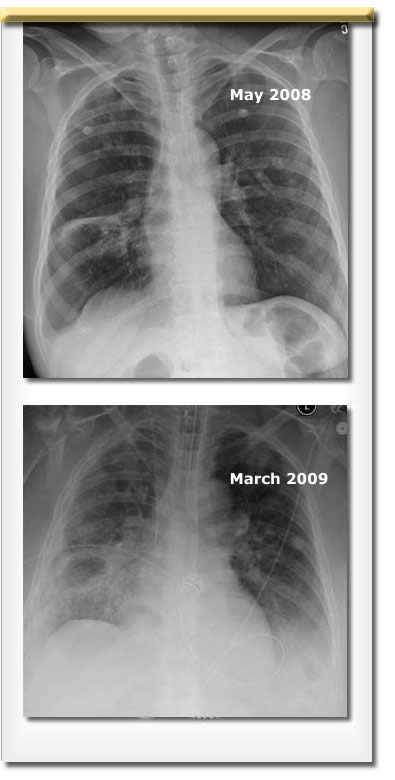 |
p>A 47 yo Native American female was admitted to the hospital in March 2009 for shortness of breath. This patient with history of closed head injury, alcoholism, IV methamphetamine use, hypertrophic cardiomyopathy, and chronic renal insufficiency had previously been hospitalized in May 2008 for abdominal pain, nausea, and vomiting. During hospitalizations at the time she had been noted to have cavitary lung disease (see upper CXR at left) and cough. Symptoms appeared to respond to clindamycin and levofloxacin; it was thought that perhaps she may have had an aspiration pneumonia. In late May 2008 (after hospital discharge) a Quantiferon-TB Gold test was performed and was reported as positive. Two sputa obtained in July 2008 were negative for AFB smear and culture. The patient exhibited a tendency to be non-compliant with medical follow-up and was jailed one or more times in the interval prior to her current hospitalization. Her March 2009 hospitalization occurred after she became increasingly short of breath. She complained of a several week long worsening of respiratory symptoms including cough prior to seeking medical care. At the time of her ER presentation she was described as smelling of alcohol but to not appear to be in distress. Examination was notable for clear lung fields and a harsh grade III/VI systolic ejection murmur. Laboratory data included WBC 11.4, Hgb 10.6, creatinine 2.5 (her baseline), and results of ABG on room air were pH 7.35, pCO2 28, pO2 72, O2Sat 97%. HIV antibody was "indeterminate." CXR is at lower left. She was begun on broad spectrum antibiotic therapy with ceftriaxone, clindamycin, and azithromycin. Sputum cultures grew Staphylococcus aureus, Streptococcus pneumoniae, and Group B streptococcus. The patient developed signs and symptoms of alcohol withdrawal, was treated with sedation, and became obtunded necessitating endotracheal intubation to protect her airway. To further evaluate her cavitary lung disease she underwent bronchoscopy. Multiple specimens were submitted for laboratory analysis. |
||
What was the cause of this patient's illness? |
|||
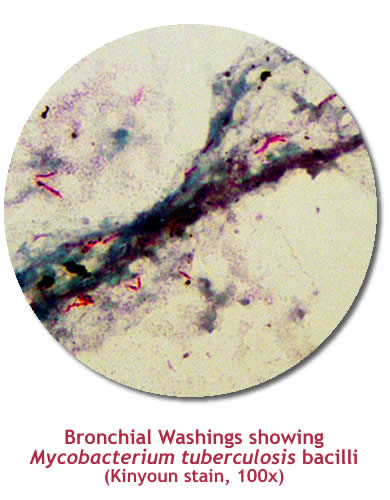 |
This patient had cavitary lung disease secondary to Mycobacterium tuberculosis. Smears of bronchial washings were loaded with AFB (see image at left) and AMPLICOR MTB test (AFB DNA PCR) on these specimens was positive for M. tuberculosis complex. Cultures subsequently grew Mycobacterium tuberculosis. Upon receipt of the smear results the patient was begun on therapy with INH, rifampin, pyrazinamide, and ethambutol. Her antibiotic therapy also included cefazolin for treatment of possible superinfecting organisms as had been isolated. She was successfully extubated after several days of mechanical ventilation and regained her baseline mental status. HIV viral load by PCR and blood cultures were negative. This patient clearly had multiple risk factors for tuberculous infection including alcoholism, IDU, imprisonment, and her ethnic background. Given the nature of her disease (cavitary, pulmonary), the smear findings (laden with organisms), and the chronicity of illness, she likely had been highly infectious for an extended time prior to institution of appropriate infection prevention precautions. The differential provided in the preceding vignette offered other plausible diagnoses. Wegener's granulomatosis can present with cavitary pulmonary nodules, and the renal insufficiency might have suggested that diagnosis. ANCA titers were negative making that disease less likely. Staphylococcus aureus may indeed have contributed to superinfecting illness. IDU associated right sided Staph aureus endocarditis with septic pulmonary emboli could have caused a similar radiographic picture. The chronicity of illness would not be typical however. Rhodococcus equi can cause pulmonary disease in immunocompromised individuals, particularly those with HIV/AIDS. Talc granulomatosis is a complication of IDU occurring when users inject solutions containing crushed oral tablets in which talc is used as filler. Definitive diagnosis requires demonstration of refractile foreign material in pulmonary granulomas. The negative AFB smears and cultures in July 2008 may have confounded those evaluating the patient at the time. The reference laboratory performing those tests advised interpretation of the results with caution because of extremely small volume specimens. The positive Quantiferon-TB Gold test of May 2008 suggested the possibility of tuberculous disease as this test can be an aid in diagnosing disease due to Mycobacterium tuberculosis.
Ref: Guidelines for using Quantiferon-TB Gold test for detecting Mycobacterium tuberculosis infection, United States, MMWR, Vol 54, No. RR-15, December 16, 2005 |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||